Learning how your joints function and what happens when your arthritis symptoms flare up can help you to understand your condition and make it easier to live with.
We have already seen how arthritis is a disease that causes pain and inflammation in the joints. It doesn’t matter which type of arthritis you have been diagnosed with, if it is not managed properly you will usually end up in a certain amount of pain and may have problems getting around and doing certain things. That said, the two major types of arthritis, osteoarthritis and rheumatoid arthritis, are actually quite different in terms of:
- their symptosm
- the rate at which they develop
- the people they affect
- the way in which they are treated
These differences arise because what’s actually going on in the joints is very different. Although both conditions involve the breakdown of cartilage in the joint, osteoarthritis is due to age related changes in which the cartilage becomes thinner in some joints, and the joint becomes less cushioned, whereas rheumatoid arthritis is related to a problem with the body’s own immune system.
Osteoarthritis occurs when the cartilage starts to disappear and the lubricating (synovial) fluid loses its protective cushioning properties.
Osteoarthritis
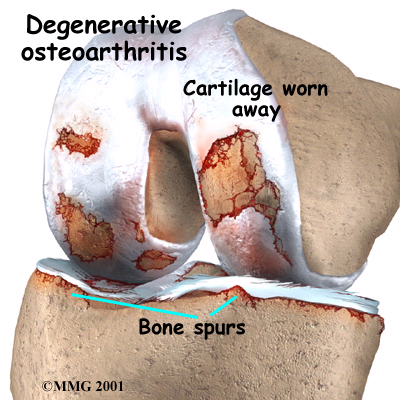
Osteoarthritis is also known as degenerative arthritis, because the cartilage that protects the bone gradually gets worn away (or degenerates). If the cartilage wears away completely then the ends of the bones can end up rubbing together, which can be extremely painful.
At one stage, scientists believed that osteoarthritis was a natural (and inevitable) consequence of getting older, but we now know this to be untrue. The real story is probably much more complicated. Although it is true that the older you get, the more worn out your joints become, not everyone of a certain age automatically develops arthritis. It is more likely that osteoarthritis can be put down to changes taking place in the miscroscopic structure of the joints. These changes may start with the cells that make cartilage. The changes that go on in your joint(s) if you have osteoarthritis usually happen in a certain order.
- The cartilage in the joint roughens and becomes worn down (and may disappear altogether).
- Tiny cracks may start to appear in the cartilage.
- Extra bone is laid down to replace the damaged or lost cartilage. The bone underneath the cartilage thickens and grows outwards.
- The amount of bone laid down far exceeds the quantity that is actually needed to replace the damage cartilage.
- Bony outgrowths (called osteophytes) start to form along the damaged joint.
- Fragments of bone may break off into the joint, which cause the joint to become inflamed and swollen (and painful_.
- The synovium starts to produce more synovial fluid than usual, which adds to the swelling in the joint.
- The loss of cartilage, the wearing of bone and the bony outgrowths can all start to change the shape of the joint. This forces the bones out of their normal position and causes deformities.
Rheumatoid Arthritis
A case of mistaken identity
Rheumatoid arthritis can be traced back to a malfunction in the immune system. The body produces antibodies that attach the cells of the joint lining (the synovium) because it mistakes it for a foreign invader, making it painful, unstable and deformed.
At the moment, no-one knows exactly what causes them but the more we understand autoimmune diseases, the easier they will be to treat and even prevent. At the moment, however, there are some gaps in what we know.
The immune response
So what are antibodies and what do they do? Antibodies are made by white blood cells called B-lymphocytes. They can be thought as Y-shaped structures, with a special region at the tip that recognises and attaches to specific foreign substances, called antigens. Once it has bound to the antibody, the antigen is neutralised so that it is no longer harmful. This process is known as immune response.
Of course, if the immune response is triggered inappropriately, perfectly healthy and harmless cells may become damaged. This is what happens in the joints when autoantibodies are made in people with rheumatoid arthritis.
Our blood is made up of three types of cell: white blood cells, red blood cells (which help to form blood clots). White blood cells are a key part of the body’s defence mechanism against infection.
How does autoimmunity cause inflammation and pain?
Rheumatoid arthritis usually progresses in three distinct stages:
- The synovium swells up and becomes inflamed as so-called inflammatory cells in the blood (specialised cells that are responsible for controlling inflammation) flock to the place where they are needed (i.e. the joint). This causes pain, warmth, redness and stiffness.
- The inflammatory cells in the synovium grow very rapidly, which causes the synovium to thicken and swell together.
- The inflamed cells then start to break down the bone and cartilage of the joint, often causing the joint to lose its shape and become unstable to move as it once did.